Healthcare providers are under increasing pressure to optimize revenue cycle management (RCM) processes, reduce operational costs, and improve the overall quality of their services. AIS aims to help solve these problems at scale by applying hyper-automation software, such as robotic process automation (RPA), designed to help organizations optimize their revenue cycles, increase productivity, and reduce costs. Our technical services are augmented and enhanced with revenue cycle management experts who consult our clients and delivery teams on how to utilize robotic process automation and other workflow solutions to capture greater revenue per visit, reduce claim denials, and keep up with an ever-increasing demand of claims to process.
An expense is the cost of providing care to a patient. An uncovered expense is a liability that grows more significant with each passing day. The longer a healthcare accounts receivable ages, the greater the burden of carrying it becomes. Submitting claims, and often re-submitting them, drains time and money from a healthcare organization. Additionally, it involves very mundane, repetitive processes that deal with complex medical codes that frequently change, adding “brain drain” to a healthcare system’s human capital and leading to errors and non-compliance.
Hyperautomation solutions help improve efficiencies and increase revenue by using programmed software “robots” to watch a human user complete a routine business task or process, then subsequently execute the same task or process. Additional capabilities can be incorporated such as the application of generative artificial intelligence algorithms, large-language models, or machine learning to further improve results.
It is helpful to use a process advisor tool to automate rules-based activities within the revenue cycle process by observing and recording manual steps completed by human users, and subsequently providing insights for improvement opportunities and return on investment information for the automation. When used in healthcare, these capabilities allow care providers to measure their return on investment in RPA in terms of key performance indicators like improvements in days to code and coding cost per account.
Reduce Operating Costs
With RPA, healthcare organizations automate entire end-to-end processes with humans typically only managing exceptions. From electronic health records to patient payment portals, RPA automates functions across a healthcare organization’s systems, allowing them to use and deploy their resources more efficiently. Instead of paying for teams of employees to execute end-to-end RCM processes, why not program intelligent bots to take care of repetitive work and let employees help design and manage the bots?
In most cases, properly applied intelligent bots complete five to eight times the amount of work per minute than what could be completed manually. These systems also can work around the clock, repeating processes without fail or rest, thereby lessening the human and financial resources required.
RPA often costs around $10,000-$13,500 per single-purpose bot, in comparison with human employees performing the same tasks for $40,000 – $55,000+ annually or more. For more sophisticated uses, the cost can significantly increase due to the need for coordination across multiple lines of business.
Increase Collections and Decrease AR Days
In RCM, human errors are often to blame for aging receivables. Payers and managed care plans commonly reject claims due to insufficient or improper documentation, delaying payment with each denial. RPA can eliminate human error and improve the accuracy of data entered, which increases the speed with which payment is collected. Further, unlike humans, each of whom may process a claim differently, an organization can immediately implement a change across the entire organization by revising the rules for automated tasks.
Common Use Cases
There are many ways to use hyper-automation in RCM. McKinsey & Company found that more than one-third of tasks in the healthcare industry could be automated, increasing efficiency throughout organizations. It’s particularly challenging in the healthcare industry to keep track of frequent medical code changes, procedure billing requirements, and federal or state regulations. Leveraging hyper-automation reduces the manual effort needed to complete the onerous and repetitive tasks involved with medical billing, along with the management of rules-based activities supporting them.
Below are examples of common use cases for using hyper-automation to improve RCM.
Missing/Incorrect NPI Numbers for Referring Physicians
Let’s look at an example where robotic process automation (RPA) can be used to address missing/incorrect National Provider Identifier (NPI) numbers for referring physicians. Such errors often impact coding; RPA can be used to identify all errors, query the NPI database, and scrub referring provider data, submitting more accurate information would improve collections. In addition to keeping claims flowing, RPA also frees clinicians and providers from hours of administrative work, allowing them to see more patients, thereby generating additional revenue.
Claims Status
Instead of having an employee visit a payer’s website for the status of a claim, we can leverage RPA to check that same site. An automated process can assess the information needed to receive payment, pull that information from connected systems, and then re-submit the claim. No team members would have to touch the claim in this example.
Other Common RCM Scenarios
- New patient appointment requests.
- Patient pre-arrival and arrival.
- Claim denials.
- Credit balances.
- Medically unlikely edits.
- Billing inquiries.
- Code changes.
Our Approach
AIS is an IT consultant and implementation services firm specializing in digital transformation solutions including intelligent process automation and is among Microsoft’s top global partners in this technology domain. There is a link provided at the bottom of this post to an open source, technical white paper my esteemed colleagues at AIS wrote with Microsoft to serve as a blueprint to administering a low-code intelligent automation platform at scale titled, “Administering a low-code intelligent automation platform”.
The combination of AIS’s top automation software architects working with clinical IT experts and revenue cycle management methodologies from AIS’s strategic healthcare partner, ReMedi Health Solution’s, deliver a comprehensive solution. ReMedi’s revenue cycle enhancement methodologies and domain experts help us improve healthcare accounting operations to work more seamlessly and improve cash flow, while also assuring full compliance and growth in revenues over the long term. Their leadership and staff are clinicians by trade; many are MDs or spent years working in healthcare before becoming services consultants.
Health system operational workflows encompass the complex processes that govern patient admission, diagnosis, treatment, and follow-up. These workflows involve multiple stakeholders, including doctors, nurses, administrative staff, and support personnel, all working together to ensure patients receive the best possible care.
Understanding these clinical workflows and aligning them with technology isn’t just about modernization; it’s about enhancing patient outcomes, reducing costs, and increasing the overall efficiency of healthcare delivery. As technology improves, the potential to transform healthcare workflows and, ultimately, patient care increases exponentially. RPA’s ability to remove the burden of repetitive tasks from staff holds great potential for increasing efficiency in the healthcare setting.
Our experienced industry practitioners work together to ensure each individual component of the revenue cycle is performing properly and that bottlenecks, manually intensive work, and errors are reduced.
This approach helps to avoid programming bots alone without considering where process adjustments and improvements can be made to further improve a specific process or task. Combining a deep understanding of the human element, the RCM business processes themselves and brilliant software architects bring comprehensive solutions that increase the value delivered. In addition, this ensures that as payment models inevitably change, the healthcare clients we serve keep up with the pace.
From ACOs to value-based purchasing, to other evolving or novel models that emerge, our experts will make sure our clients remain ready for the dynamic nature of healthcare economics.
Here is a high-level overview of a general approach we would use with a brief description of what is entailed.
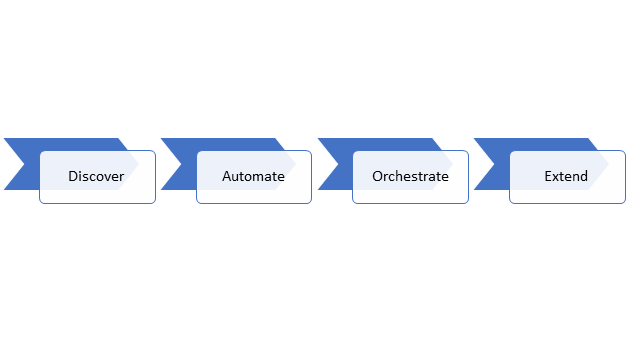
Figure 1: Hyperautomation Approach
- Discover: Our team of clinical, administrative, and technical experts collaborates with a healthcare system to pinpoint process improvement opportunities through the application of RPA and other hyper-automation capabilities.
- Automate: Next, we design, build, and rapidly deliver automation solutions and RPA bots anchored by a management program and infrastructure to support them. Our onshore software architects are supported by AIS’s secure offshore development center in Hyderabad, India to provide economical engineering based on the Architect’s design and architecture plans to control development costs. Our teams use existing tooling, accelerators, and reference templates that AIS has developed or our partners like Microsoft have available to further decrease development time and efforts. During the development lifecycle, our teams establish specific patterns, templates, and a common set of artifacts for future use. You can read more about this in the white paper I mentioned earlier linked below.
- Orchestrate: Once RPA bots are in use, we enable healthcare teams to actively refine RPA capabilities, support ongoing and changing industry conditions and medical codes, and support active bots. We then capture results from improvements made to examine the financial and qualitative impacts of the bots.
- Extend: Once the first set of RPA bots are live, demonstrating value and return on investment, more bots can be programmed to eliminate additional RCM processes as part of an integrated strategy and supporting program.
Business Impact
Our RPA solutions drive deep impact for healthcare revenue cycle management by automating critical functions such as claims processing, eligibility verification, and prior authorization. This leads to streamlined operations, reduced error risks, and accelerated cycle times, significantly enhancing the efficiency and accuracy of healthcare services. There are non-financial impacts derived as well, including the following:
Increased Revenue:
- Speed up claims processing.
- Reduce the risk of lost revenue.
- Expand service capacity to more patients.
Improved Compliance:
- Adhere to the highest security and compliance standards.
- Ensure accurate and consistent completion of tasks.
- Reduce exposure to risks and ensured compliance with regulatory requirements.
Enhanced Decision-Making:
- Provide insights for clinical operation optimization.
- Improve patient outcomes through data-driven strategies.
Reduced Administrative Burden:
- Automate routine tasks.
- Enable clinicians to focus more on patient care.
Our team of experts works closely with healthcare organizations to understand their specific needs and develop tailored solutions that optimize their revenue cycle processes. Get in touch if you would like to talk with us or learn more about how our Robotic Process Automation Solution for Healthcare RCM can help your organization.
About AIS
For over 40 years, AIS has helped hundreds of global enterprises optimize their technology investments to overcome IT challenges and achieve business goals. We deliver digital and cloud transformation solutions that help commercial and federal enterprises improve business results by migrating to the cloud, modernizing apps, and using data intelligence.
Website: https://www.ais.com/about/
About ReMedi Health Solutions
ReMedi Health Solutions is a nationally recognized, physician-led healthcare IT consulting firm specializing in peer-to-peer, physician-centric EHR implementation and training. ReMedi is a clinically driven company committed to improving the future of healthcare.
Website: https://www.remedihs.com/
References
Administer and govern a low-code intelligent automation platform whitepaper: Enterprise deployment for RPA and more in Power Automate: https://powerautomate.microsoft.com/en-us/blog/administer-and-govern-a-low-code-intelligent-automation-platform-whitepaper-enterprise-deployment-for-rpa-and-more-in-power-automate/
White Paper (Enterprise Deployment for RPA and more in Power Automate): https://aka.ms/autocoeadminwhitepaper






